2025 Annual Research Forum: Resident WinnerQuantifying Savings from Implementing the Brain Injury Guidelines at a Level 1 Trauma CenterFirst Author: Ryan Johnson, MD, MS; University of Texas at Houston

Co-Authors: Mary-Kate Gorlick, Carrie Bakunas, Benjamin Cooper, and Kunal Sharma Background: Traumatic brain injuries (TBI) account for significant emergency department (ED) resource utilization, often involving costly imaging studies, neurosurgical consultations, prolonged ED stays, and inter-facility transfers. Many patients with mild TBIs, particularly those with isolated intracranial hemorrhages, are managed conservatively without complications. The Brain Injury Guidelines (BIG) offer a standardized algorithm to stratify patients into risk groups, allowing clinicians to safely avoid unnecessary interventions for low-risk patients (BIG 1 criteria). While the BIG algorithm has demonstrated safety and efficacy in clinical studies, its financial implications remain understudied. This research quantifies potential cost savings from implementing BIG criteria at a level one trauma center, focusing on imaging, LOS, and transfer-related expenses. Methods: We retrospectively reviewed data from a cohort of 2,411 patients with TBI presenting to the ED in 2023. A random sample of 225 patients underwent detailed chart review to identify those meeting BIG 1 criteria. For these patients, actual resource utilization—including CT imaging, ED LOS, and inter-facility transfer costs—was compared to hypothetical usage based on BIG recommendations. Cost calculations were based on published cost estimates from ED literature. Avoidable costs for each resource were aggregated to determine potential annual savings. Results: Of the 225 patients reviewed, 36 (16%) met BIG 1 criteria. Consistent with prior studies, these patients experienced no deaths or neurosurgical interventions, reinforcing the safety of the BIG algorithm. On average, patients meeting BIG 1 criteria underwent 1.94 CT scans per ED visit. Retrospective application of BIG guidelines indicated that 362.6 CT scans could have been avoided annually, resulting in potential savings of $504,078. LOS analysis revealed that BIG 1 patients arriving de novo (not transferred) had an avoidable ED stay of 4.1 hours, contributing to an estimated annual savings of $78,140. Transferred patients meeting BIG 1 criteria had an average avoidable LOS of 11 hours, yielding an additional $118,495 in potential savings. Among the transferred patients, 36% (13/36) met BIG 1 criteria, and over half (54%) did not require any specialty consultations other than neurosurgery. Avoiding these transfers could have saved $52,500 annually in transportation costs. 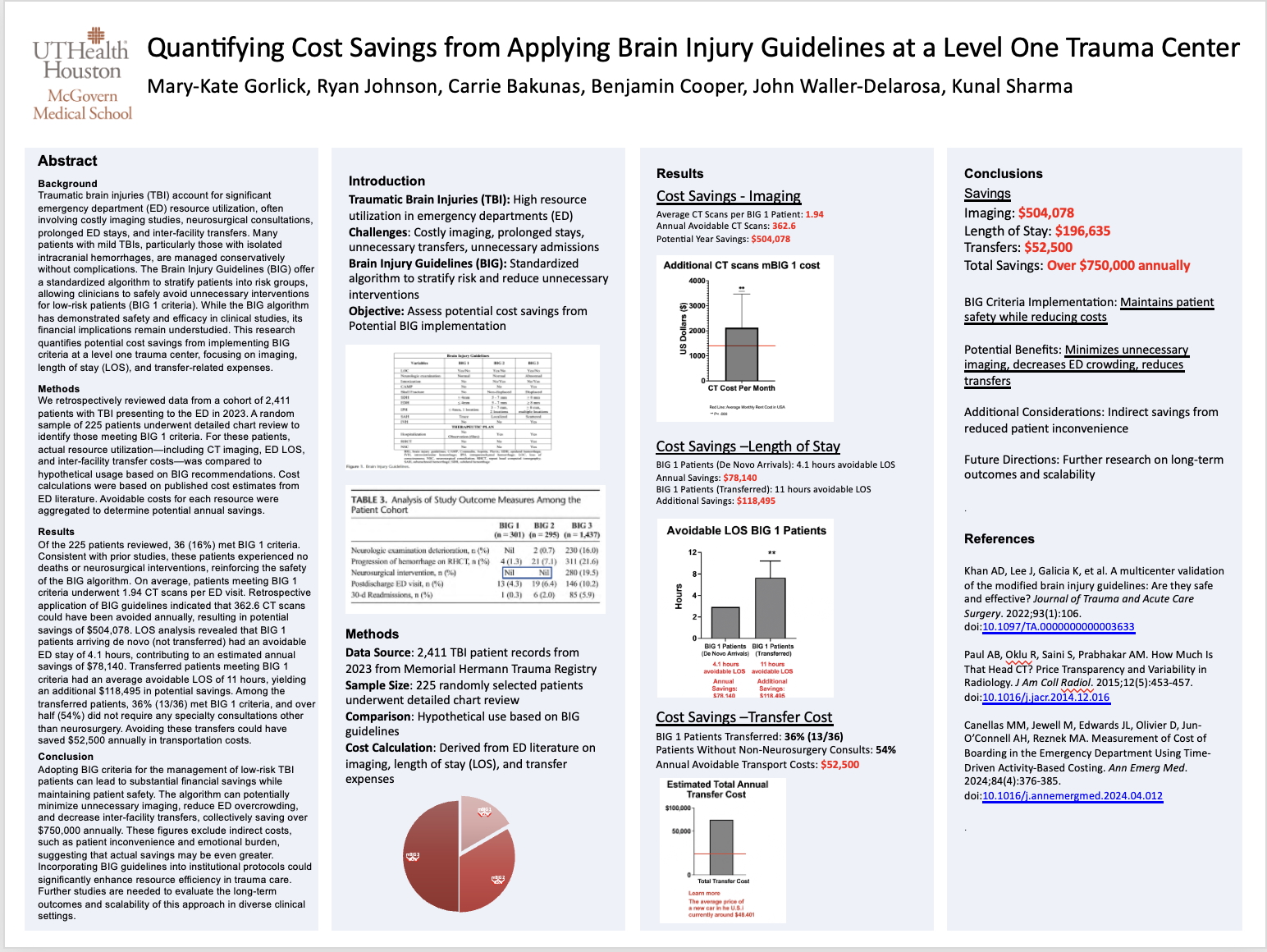 Acknowledgements: University of Texas at Houston Medical Incident Reporting System
|
