2025 Annual Research Forum: Student Winner
Risk of Coagulopathies in Severely Burned vs Non-Severely Burned Patients Lacking Lower Extremity Trauma
First Author: Lt. Rochak Khatri; University of Texas Medical Branch John Sealy School of Medicine
 Co-Authors: Christina Rios; Amina El Ayadi, PhD; Steven Wolf, MD Co-Authors: Christina Rios; Amina El Ayadi, PhD; Steven Wolf, MD
Background: Burn injuries can affect coagulation in patients during both the acute and recovery phases of their injuries. Virchow's triad of hypercoagulability, endothelial damage, and venous stasis provides insight into the pathophysiology of adverse coagulopathies in burn patients. While few studies have examined the risk of coagulopathies based on the severity of the burns, traumatic injuries that may significantly contribute to coagulopathies were not excluded. This study looks to evaluate whether severe burns patients without lower extremity trauma are at an increased risk of developing coagulopathy complications when compared to non-severe burns patients.
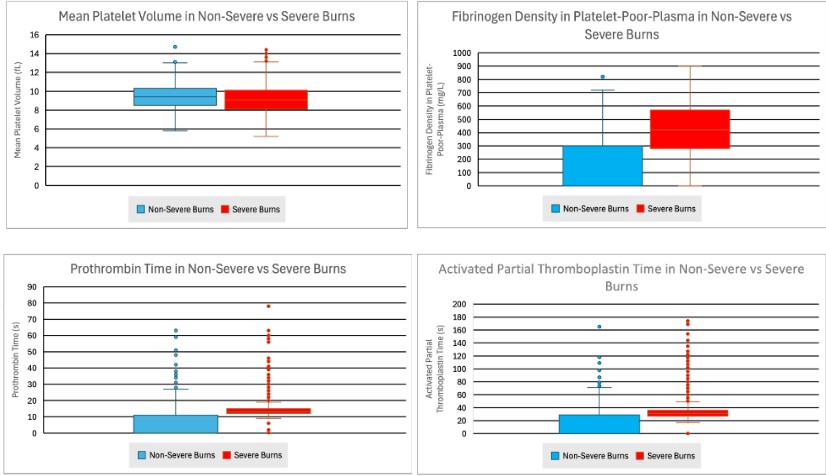
Methods: This retrospective study utilizes the TriNetX database to evaluate 157,567 burn patients from 90 health care organizations (HCOs) globally from 2005-2025. Burn injuries were categorized as severe if involving 30% or more of total body-surface area (TBSA) and non-severe if involving less than 30% TBSA. Traumatic injuries of the lower extremities were excluded for both groups to prevent immobilization from non-burn injuries to influence outcomes of hypercoagulability. Severe burns were defined using the ICD-10-CM codes T31.3 -T31.9. Non-severe burns were defined using ICD-10-CM codes T31.0 - T31.2. Cohorts were propensity matched with demographic covariates and ICD-10-CM codes were used to compare outcomes of venous thromboemboli (I73), arterial thromboemboli (I74), pulmonary emboli (PE) (I26), acute deep vein thromboses (I82.409), and coagulopathies (D65-D69) between the groups. Laboratory values for platelet volume (TNX:9019), prothrombin time (PT) (TNX:9033), activated partial thromboplastin time (aPTT) (TNX:9031), fibrin D-dimer FEU (LNC:48065-7), and fibrinogen in platelet-poor plasma (PPP) (LNC:3255-7) were also compared between the two groups.
Results: The severe burns cohort had a 2.774 times higher risk of developing venous thromboemboli, a 2.188 times higher risk of developing arterial thromboemboli, a 3.236 times higher risk of developing pulmonary emboli, a 2.976 times higher risk of developing acute DVT, and a 2.066 times higher risk of developing unspecified coagulopathies compared to the non-severe burns cohort. These data were all significant with a P<0.05. Mean platelet volume in the severe burns cohort was significantly reduced compared to the non-severe burns cohort with P<0.05. Mean PT and aPTT times were significantly prolonged in the severe burns cohort compared to the non-severe burns cohort with P<0.05. Mean concentrations of fibrin D-dimer products and fibrinogen density were significantly elevated in the severe burns cohort compared to the non-severe burns cohort with P<0.05.
Conclusions: Findings indicate a significant correlation in the development of coagulopathy complications in severe burns patients without lower extremity trauma when compared to non-severe burns patients. Significantly reduced platelet volume, increased PT and aPTT times, and elevations in D-dimer and fibrinogen concentrations support the findings of underlying coagulopathies in this cohort. Increased risk of coagulopathies should influence acute management of severe burn patients lacking trauma.
|

 Co-Authors: Christina Rios; Amina El Ayadi, PhD; Steven Wolf, MD
Co-Authors: Christina Rios; Amina El Ayadi, PhD; Steven Wolf, MD